Contents
HOTCOMP Paid $3,280,046 in dividends since 2008
Common Industry Hazards for HOTCOMP Hospital’s
Coronavirus (COVID-19) frequently asked questions for employers
PPE in Healthcare: How to Prevent Exposure and Contamination
HOTCOMP Safety Committee Welcomes Christi Reeves
Texas Mutual’s e-Learning ADVANTAGE
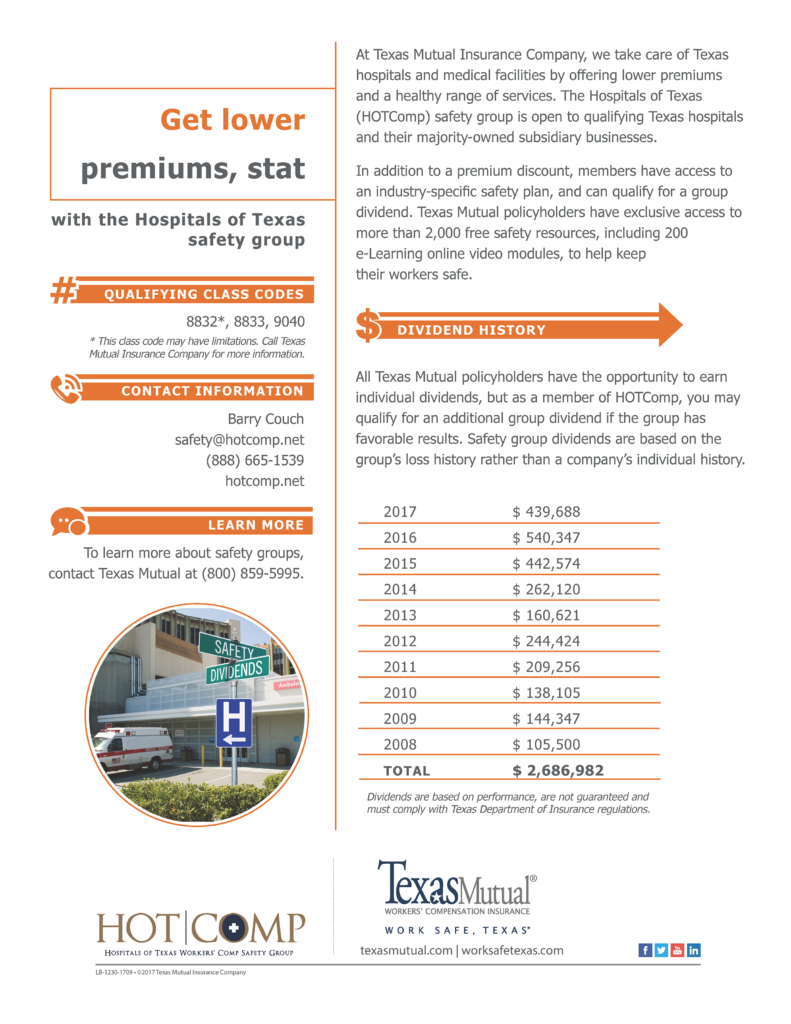
HOTCOMP Paid $3,280,046 in dividends since 2008
Common Industry Hazards for HOTCOMP Hospital’s
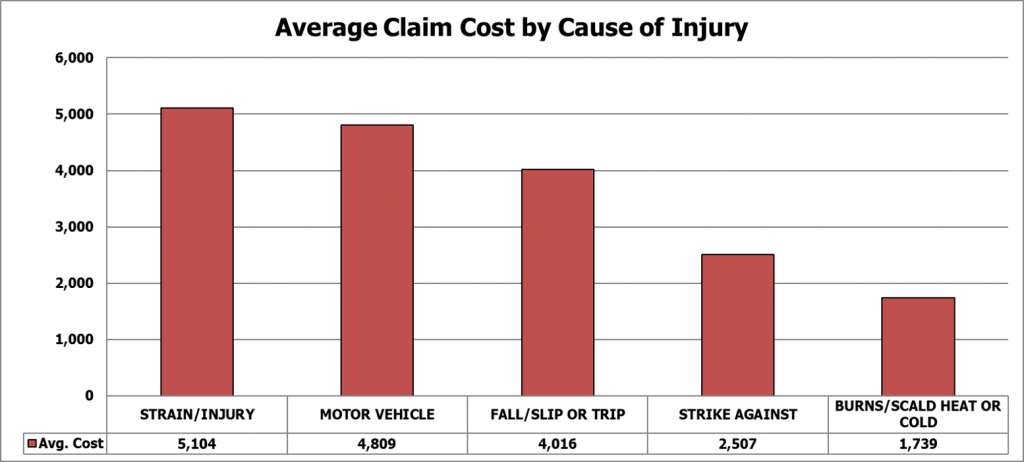
Loss Analysis:
The most common causes of injury among HOTCOMP safety group members for the past five years were cut/puncture/scrape, fall/slip or trip, strain, miscellaneous causes and being struck by objects.

During this time, the causes of injury with the highest average claim cost were strain, motor vehicle collision, fall/slip or trip, strike against and burn.
Common Industry Hazards:
A list of activities or situations that contributed to the safety group’s injuries is provided below in order to raise awareness of common hazards within the industry. After reviewing this list, download the Common Control Strategies document from the Texasmutual.com Safety Resource Center to learn how to protect your employees from these hazards.
Cut/Puncture/Scrape:
- Cuts from sharp medical instruments
- Improper handling and disposal of needles and other sharps
- Contact with needles while handling laundry
- Broken glasses and bottles
Fall/Slip or Trip:
- Slippery floors from spills, wet areas, grease, and food debris
- Poor housekeeping
- Slips/falls at door entries due to inclement weather
- Falls from improper use of ladders or step stools
Strain:
- Lifting of patients (i.e. transfers from wheelchairs, beds, toilets, showers)
- Handling aggressive patients
- Lifting food trays
- Handling laundry
- Lifting various inventory, supplies, and equipment
Motor Vehicle Collision:
- Excessive speed
- Driving while fatigued
- Increased severity due to lack of seatbelt use
- Distracted driving including texting or talking on cell phone while driving
Struck By:
Coronavirus (COVID-19) frequently asked questions for employers
According to the U.S. Centers for Disease Control and Prevention (CDC), the risk of infection of COVID-19 is currently low, even for most workers. However, as an employer you may face questions and concerns, which we want you to feel prepared to address.
Workers’ compensation claims related to COVID-19
Are COVID-19 claims compensable?
Texas Mutual will investigate each COVID-19 claim on a case-by-case basis. Our team of claim specialists will investigate the facts of each case and evaluate whether an employee’s illness related to COVID-19 occurred during the course and scope of employment. As with any claimed occupational disease, the medical evidence will be important to the compensability determination.
Certain types of employment or circumstances specific to your business may carry a higher risk of COVID-19 exposure than others, and we will carefully weigh all factors presented in each potential COVID-19 claim before making any compensability determination.
If COVID-19 becomes a pandemic, and an employee claims that he or she contracted it at work, how will those claims be handled?
As explained above, we will evaluate each COVID-19 claim on a case-by-case basis and consider all factors to determine whether the exposure occurred in the course and scope of employment. However, the more widespread COVID-19 becomes, the more difficult it may be for the employee to show that it is work related rather than an ordinary disease of life to which the general public is
exposed.
When should I report a claim for suspected or diagnosed COVID-19?
Report all claims that you suspect may be work related immediately. We have a team of highly trained claim specialists dedicated to handling any claims involving COVID-19 that we may receive.
How do I report suspected COVID-19 claims?
Please report suspected COVID-19 cases by calling us at (800) 892-5246, submitting the claim online, emailing claims@texasmutual.com or faxing the claim to (877) 404-7999.
If my business must require employees to work from home, what happens if they get injured while working from home?
We will investigate and evaluate any claimed injury that occurs while working from home just as we would a claim in the workplace. We will determine whether the injury arose from the employment and occurred while furthering the business of the employer. For example, an injury occurring while the employee was setting up her remote workstation likely would be compensable. An injury that occurred while the employee was walking downstairs first thing in the morning likely would not be considered compensable.
COVID-19 in your business or among employees
What are the symptoms of COVID-19?
Reported illnesses have ranged from mild symptoms to severe illness and death for confirmed cases of COVID-19 disease. The following symptoms may appear two to 14 days after exposure:
- Fever
- Cough
- Shortness of breath
What should I do if I suspect one of my employees has been exposed to COVID-19?
If you suspect an employee has been exposed:
- Instruct the employee to stay home and not come to work.
- Advise the employee to contact their health care professional if they have developed symptoms and have been in close contact with a person known to have COVID-19, or if the employee has recently traveled from an area with widespread or ongoing community spread of COVID-19.
If you or the employee reasonably believes that the COVID-19 exposure could be work related, please report a claim by calling us at (800) 892-5246, submitting the claim online, emailing claims@texasmutual.com or faxing the claim to (877) 404-7999.
If you have employees with upcoming travel plans, the CDC recommends these additional preventative measures:
- Do not travel while sick.
- Supplies of hand sanitizer, tissues, and other hygiene products may be limited, so consider
bringing them with you. - Pay attention to your health during travel and for 14 days after you leave.
Prevention and the spread of COVID-19
How does COVID-19 spread?
There are several ways the coronavirus can spread:
- Person-to-person spread
- The virus is thought to spread mainly from person to person.
- Between people who are in close contact with one another (within about six feet).
- Through respiratory droplets produced when an infected person coughs or sneezes.
- These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
- Spread from contact with infected surfaces or objects
- It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads.
- Can someone spread the virus without being sick?
- People are thought to be most contagious when they are most symptomatic (the sickest).
- Some spread might be possible before people show symptoms. There have been reports of this occurring with this new coronavirus, but this is not thought to be the main way the virus spreads.
My employees have a heightened risk of COVID-19 exposure. Are there basic safety tips we should follow?
We encourage you to visit the CDC website for the most up to date information on coronavirus. Below are basic recommendations.
The CDC recommends that everyone use simple preventive actions to help prevent the spread of respiratory diseases, including:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
- Follow the CDC’s recommendations for using a facemask.
- The CDC does not recommend that people who are well wear a facemask to protect themselves from respiratory diseases, including COVID-19.
- Facemasks should be used by people who show symptoms of COVID-19 to help prevent the spread of the disease to others. The use of facemasks is also crucial for health workers and people who are taking care of someone in close settings (at home or in a health care facility).
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom, before eating, and after blowing your nose, coughing, or sneezing.
- If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol. Always wash hands with soap and water if hands are visibly dirty.
More information
Where do I get more information?
Health care organizations across the globe are working hard to arm everyone with knowledge they need to protect themselves. Here are some links to credible organizations that offer more information:
- Centers for Disease Control and Prevention
- National Institute for Occupational Safety and Health
- Occupational Safety and Health Administration
- World Health Organization
More information about coronavirus and prevention can be found on the Texas Mutual blog.
PPE in Healthcare: How to Prevent Exposure and Contamination
American Society of Safety Professionals
When people think about personal protective equipment (PPE), they may think of hard hats, surgeon putting on surgical gloves before operation steel-toe boots and protective eyewear. In the healthcare industry, however, PPE takes on a different meaning and purpose. In many work settings, PPE is used to protect workers from potential injuries. In healthcare, the primary purpose of PPE is to protect doctors, nurses and others from illness as they work with patients.
More than 18 million Americans work in the healthcare industry and without the proper PPE, these workers are putting their own safety, health and well-being and that of the public at risk.
“PPE is very much an active control, where the employee has to recognize the need for it, find, get it, put it on and ensure that it is effective,” says Cory Worden, CSP, safety advisor for the City of Houston Department of Health.
In most cases, safety professionals are told to start at the top of the hierarchy of controls as they address workplace hazards. In healthcare, however, PPE may be the best, and in some cases, only option for protecting doctors, nurses and others from illness.
“We can’t eliminate the hazard because it’s a patient and we can’t choose our patients,” says Worden. “We can’t substitute our patients or isolate doctors and nurses from the patient with engineering controls, so the only thing that is even possible to do to keep all of those bodily fluids off of a nurse or doctor is PPE.”
These three concepts can help protect the health and safety of doctors, nurses, staff and the public.
- Develop Situational Awareness
A hospital may have hundreds of patients at any one time, many with unique ailments. This makes situational awareness critical to protecting the health of doctors, nurses, patients and the public.“A big part of this equation is doctors and nursing staff familiarizing themselves with the conditions of every patient,” says Worden. “It’s important for them to be diligent about staying up on all the patients that they’re dealing with and communicate that to everyone affected so they know what kind of PPE needs to be worn before they even set foot in a patient’s room.”
Situational awareness helps hospital staff and visitors know what PPE they need to wear around each patient, such as a gown, gloves, a face shield or a respirator. Worden notes that each patient who comes through the door is unique situation, so medical staff must assess that patient by asking several key questions:
- Does the patient present any specific hazards, other than the fact that they’re seeking healthcare?
- What is the severity of those hazards?
- What can be done to address those hazards?
For example, an ill patient may enter a healthcare facility after returning from overseas travel. In such a case, the staff must take precautions to protect the public. The patient may be given a surgical mask to prevent droplet contamination from coughing or sneezing.
It’s also important to remember that each patient’s condition is constantly changing, making communication and situational awareness throughout their stay at the healthcare facility all the more critical.
- Learn How to Don and Doff Equipment Correctly
To properly protect yourself and others in healthcare environments, you have to understand how to properly put on and take off PPE. To prevent potential exposure or contamination, staff must follow specific protocols for donning and doffing PPE before and after entering a patient’s room.“Donning and doffing is very much a diligence-based process that everyone needs to be intensely familiar with,” says Worden. “If we’re not extremely diligent in making sure everything is done properly, there will be an exposure.”
CDC offers guidance on the sequence for donning and doffing specific pieces of PPE in healthcare settings. Both actions are step-by-step processes where employees must put on and take off equipment in a specific order.
When putting on equipment, users must ensure that PPE is the proper fit, that it is taped appropriately and that there are no gaps that would allow it to be infiltrated. After the patient has been treated and medical staff move from the “hot area” or hazardous area and into the “warm area” or transition area, they should remove equipment one piece at a time.
- Properly Dispose of Equipment
Once equipment is removed, it must be appropriately discarded to prevent potential bloodborne pathogen exposure or other contamination.“With any type of contaminated waste, there is always the possibility of cross-contamination, so any medical waste has to be properly discarded and properly disposed of,” says Worden.
The waste is placed into containers that must be emptied when they are three-quarters full. State regulations dictate how disposal of medical waste is handled. The EPA encourages healthcare facilities to speak with their state EPA or state health agency for information regarding medical waste disposal.
Worden notes that in addition to PPE “sharps” such as syringes and other such medical devices are subject to specific OSHA recordkeeping requirements. He adds that hospital staff must ensure that any medical waste is safely and securely disposed of, not only for employees to avoid injuries and illnesses, but also for patients and the general public. Having used medical equipment lying around or in a location that is easily accessible endangers the health and safety of everyone in the facility.
To help medical professionals, safety professionals and healthcare facility staff, Worden developed a hazard control tracking chart, PPE assessment matrix and a frequency and severity model to help identify hazard groups, the PPE needs for each of those groups and probability and severity of specific hazards.
HOTCOMP Safety Committee Welcomes Christi Reeves
The HOTCOMP Safety Committee has added a new member Christi Reeves to our Safety Committee. Christi is the Nursing AVP at Oakbend Medical Center. We are excited for her help addressing the issues of safety in our member hospitals and what we can do to do to help make them safer workplaces.
Safety Training at Texas Mutual
Building a safer workplace is your number one way to control workers’ compensation costs. Explore resources exclusively available to you as a Texas Mutual policyholder.
Online tools and e-Learning
- Safety webinars
- Safety courses
- Online OSHA training
- Texas Mutual events
Click Here to check it out.
Your Safety Committee
The HOTCOMP Safety Committee meets twice a year to discuss the issues of safety in our member hospitals and what we can do to do to help make them safer workplaces.The majority of the Committee members are administrators and safety specialists in your fellow member hospitals. We understand that issues come up through the year. If you would like to post a question to the safety committee members as a group or individuals, please email us at safety@hotcomp.net. We will pass your questions on to the appropriate member(s).
|
Barry Couch, CEO
Program Administrator
|
Linda Rasor, CEO
Castro County Hospital
|
Gayle Cannon , Director of HR
Childress Regional Medical Center
|
|
Carol Villareal, HR Manager
Gonzales Healthcare System
|
Brian Roland, CEO
Muenster Memorial Hospital
|
Christi Reeves, Nursing AVP
Oakbend Medical Center
|
About Safety Matters:
It is our hope that this publication, in addition to Texas Mutual’s Safety Resource Center, proves a useful tool to promote safety in our members’ hospitals. The newsletter will focus on safety issues that specifically trend to our membership hospitals.
We hope to hear from you on safety issues your hospital is facing and on successful safety procedures you have implemented. It is the safety committee’s goal to create a collaborative exchange of ideas that contributes to making all of our hospitals safer which, in turn, will increase our safety group’s benefits.
Please send your ideas, questions and comments to safety@hotcomp.net.
Why Your Safety Matters:
You’re receiving this email as a member of the HOTComp safety group. The group is a joint effort between HealthSure and Texas Mutual Insurance Company.
Group members receive exclusive benefits like targeted safety resources, a discount on their workers’ compensation insurance and potential dividends based upon the safe performance of the group. HOTComp group participants have shared in over $1 million in group dividends since 2008 in addition to individual dividends from Texas Mutual.