-
Contents
- The provision of first aid by an employee who is not a licensed health care provider;
- The dispensing of prescriptions by pharmacists in retail settings;
- Non-hospital ambulatory care settings where all non-employees are screened prior to entry and people with suspected or confirmed COVID-19 are not permitted to enter those settings;
- Well-defined hospital ambulatory care settings where all employees are fully vaccinated and all non-employees are screened prior to entry and people with suspected or confirmed COVID-19 are not permitted to enter those settings;
- Home health care settings where all employees are fully vaccinated and all non-employees are screened prior to entry and people with suspected or confirmed COVID-19 are not present;
- Health care support services not performed in a health care setting (off-site laundry, off-site medical billing, for example); and
- Telehealth services performed outside of a setting where direct patient care occurs.
- Minimize the risk of COVID-19 transmission for each employee. Although the employer’s plan must account for the potential COVID-19 exposures to each employee, the plan can do so generally and does not need to address each employee individually.
- Effectively communicate and coordinate with other employers. When employees of different employers share the same physical location, each employer must effectively communicate its COVID-19 plan to all other employers. They must also coordinate to ensure that each of their employees is protected and adjust their COVID-19 plans to address any particular COVID-19 hazards presented by the other employees. This requirement does not apply to delivery people, messengers or other employees who only enter a workplace briefly to drop off or pick up items. An employer with one or more employees working in a physical location controlled by another employer must notify the controlling employer when those employees are exposed to conditions at the location that do not meet the requirements of this section.
- Protect employees who in the course of their employment enter into private residences or other physical locations controlled by a person not covered by the Occupational Safety and Health Act (OSH Act). This must include procedures for employee withdrawal from that location if those protections are inadequate.
- Limit and monitor the points of entry to the setting. This provision does not apply where emergency responders or other licensed health care providers enter a non-health care setting to provide health care services.
- Screen and triage all clients, patients, residents, delivery people and other visitors and other non-employees entering the setting.
- Implement other applicable patient management strategies in accordance with the CDC’s COVID-19 Infection Prevention and Control Recommendations.
- When an employee is alone in a room.
- While employees are eating and drinking at the workplace, provided each employee is at least six feet away from other persons or separated from other people by a physical barrier.
- When employees are wearing respiratory protection in accordance with OSHA’s respiratory protection program (29 CFR 1910.134) or the ETS.
- When it is important to see a person’s mouth (communicating with hearing impaired individuals) and the conditions do not permit a facemask that is constructed of clear plastic. In those situations, employers must ensure that employees wear an alternative means to protection, such as a face shield, if the conditions permit it.
- When employees cannot wear facemasks due to a medical necessity, medical condition or disability as defined in the Americans with Disabilities Act (ADA) or due to religious belief. OSHA has indicated that exceptions must be provided for a narrow subset of persons with a disability if they cannot wear a facemask or cannot safely wear a facemask because of a disability under the ADA. The remaining subset of people who cannot wear a mask may be exempted on a case-by-case basis as required by the ADA. In all such situations, employers must ensure that any such employee wears a face shield for the protection of the employee, if their condition or disability permits it. Accommodations may also need to be made for religious beliefs consistent with Title VII of the Civil Rights Act.
- When the employer can demonstrate that the use of a facemask presents a hazard of serious injury or death to an employee. In these situations, employers must ensure that each employee wears an alternative means of protection (for example, a face shield), if the conditions permit it. Any employee not wearing a face mask must remain at least six feet away from all other people unless the employer can demonstrate physical distancing is not feasible. Employees must resume wearing a facemask when not engaged in the activity where the facemask presents a hazard.
- A respirator to each employee and ensure that it is provided and used in accordance with the respiratory protection program; and
- Gloves, an isolation gown or protective clothing and eye protection to each employee and ensure that the PPE meets the ETS requirements.
- Limit the number of employees present during the procedure to only those essential for patient care and procedure support.
- Ensure that the procedure is performed in an existing airborne infection isolation room (AIIR), if available.
- After the procedure is completed, clean and disinfect the surfaces and equipment in the room or area where the procedure was performed.
- Telehealth;
- Telework or other remote work arrangements;
- Reducing the number of people, including non-employees, in an area at one time;
- Visual cues such as signs and floor markings to indicate where employees and others should be located, or to indicate their direction and path of travel;
- Staggered arrivals, departures, and work and break times; and
- Adjusted work processes or procedures to allow great distance between employees.
- Clean high-touch surfaces and equipment at least once a day, following manufacturers’ instructions for application of cleaners; and
- Clean and disinfect, in accordance with CDC’s Cleaning and Disinfecting Guidance, any areas, materials and equipment under the employer’s control when the employer is aware that an employee who is COVID-19 positive has been in the workplace within the last 24 hours.
- The HVAC system is used in accordance with the HVAC manufacturer’s instructions and the design specifications of the HVAC system;
- The amount of outside air circulated through its HVAC system and the number of air changes per hour are maximized to the extent appropriate;
- All air filters are rated minimum efficiency reporting value (MERV) 13 or higher, if compatible with the HVAC system. If MERV-13 or higher filters are not compatible with the HVAC system, employers must use filters with the highest compatible filtering efficiency for the HVAC system;
- All air filters are maintained and replaced as necessary to ensure the proper function and performance of the HVAC system; and
- All intake ports that provide outside air to the HVAC system are cleaned, maintained, and cleared of any debris that may affect the function and performance of the HVAC system.
Employers that have an existing airborne infection isolation room (AIIR) must maintain and operate it in accordance with its design and construction criteria. The ETS does not require installation of new HVAC systems and AIIRs. Employers should, however, consider other measures to improve ventilation in accordance the CDC’s Ventilation Guidance. This can include maximizing ventilation in buildings without HVAC systems or in vehicles.
Health Screening and Medical Management
Employers must screen each employee before each work day and each shift. Screening may be conducted by asking employees to self-monitor before reporting to work or may be conducted in-person by employers. Employers that require COVID-19 tests for screening purposes must provide these tests at no cost to the employees.
Screening
Employers must require each employee to promptly notify them when the employee:
- Is COVID-19 positive (confirmed positive test for, or has been diagnosed by a licensed health care provider with, COVID-19);
- Has been told by a licensed health care provider that they are suspected to have COVID-19;
- Is experiencing recent loss of taste or smell with no other explanation; or
- Is experiencing both a fever equal to or greater than 100.4 degrees Fahrenheit and a new unexplained cough associated with shortness of breath.
Employer Notification of COVID-19 Exposure
Employers that receive notification that a person who has been in their workplace is COVID-19 positive must complete the following requirements within 24 hours. The requirement applies regardless of whether the infected individual is an employee or a client, patient, resident, vendor, contractor, customer, delivery person, visitor or other non-employee.
- Notify each employee who has been in close contact with a COVID-19 positive individual. This requirement applies to employees who were not wearing a respirator or any other required PPE and have been in close contact with that person in the workplace. The notification must state that the employee was in close contact with someone with COVID-19, along with the date(s) that contact occurred.
- Notify all other employees who were not wearing a respirator or any other required PPE and worked in a well-defined portion of a workplace in which the positive COVID-19 person was present during the potential transmission period. The potential transmission period runs from two days before the person felt sick (or, for asymptomatic people, two days prior to test specimen collection) until the time the person is isolated. The notification must specify the dates the person with COVID-19 was in the workplace during the potential transmission period.
- Notify other employers whose employees were not wearing respirators or any other required PPE and were in close contact with the COVID-19-positive person, or worked in a well-defined portion of a workplace (for example, a particular floor) in which that person was present, during the potential transmission period (as described above). The notification must specify the dates the person with COVID-19 was in the workplace during the potential transmission period and the locations where the person with COVID-19 was in the workplace.
Notifications must not include any employee names, contact information (phone number, email address) or occupation. The notification provisions are not triggered by the presence of a patient with confirmed COVID-19 in a workplace where services are normally provided to suspected or confirmed COVID-19 patients (emergency rooms, urgent care facilities, COVID-19 testing sites, COVID-19 wards in hospitals).
Medical Removal from the Workplace
Employers are required to remove employees from the workplace when employers know that the employees:- Are COVID-19 positive, meaning that they were confirmed positive for, or were diagnosed by a licensed healthcare provider with, COVID-19;
- Have been told by a healthcare provider that they are suspected to have COVID-19;
- experiencing recent loss of taste or smell, with no other explanation;
- Are experiencing both fever (≥100.4° F) and a new unexplained cough associated with shortness of breath; or
- Are required to be notified by the employer of close contact in the workplace to a person who is COVID-19 positive, UNLESS the employee has been fully vaccinated against COVID-19 (i.e., two weeks or more have passed following the final dose), or had COVID-19 and recovered within the past three months, AND the employee does not experience the symptoms listed above.
Employers must remove these employees from the workplace and keep these employees removed until the employees meet return-to-work criteria based on guidance from a licensed health care provider or applicable guidance from the CDC, unless state or local public health authorities specify a longer period of removal.
For cases when employee infection is not confirmed or diagnosed, employers may allow employees to return to work immediately after a negative COVID-19 polymerase chain reaction (PCR) test. The PCR test must be provided at no cost to the employees.
Employers may choose to go beyond the minimum requirements of the ETS. For example, they may choose to remove employees who (1) are experiencing symptoms other than recent loss of taste and/or smell or fever coupled with new unexplained cough and shortness of breath, (2) were exposed to a COVID-19-positive person outside of the workplace, or (3) were notified by a state or local public health authority to quarantine or isolate. Although the ETS does not require removal in those situations, the state or local public health authority may impose separate obligations or the employer might choose to remove employees in those circumstances, above and beyond what is required by this ETS.
Medical Removal Protection Benefits
The ETS creates medical removal protection (MRP) benefits for employees who are required to quarantine because of COVID-19. MRP benefits require employers to continue paying removed employees the same regular pay and benefits the employee would have received had the employee not been removed. The benefits must continue until employees meet the return-to-work criteria or the medical removal expires.
Obligations to pay the removed employee depend on the size of the employer:
- Employers with 10 or fewer employees on the date that the ETS becomes effective are not required to maintain pay for removed employees.
- Employers with fewer than 500 employees must pay the employee’s regular pay, up to $1400 per week, for the first two weeks that the employee is removed. Beginning in the third week, if the employee’s removal continues that long, the employer must pay two-thirds of the same regular pay the employee would have received if working, up to $200 a day (equivalent to $1000 per week in most cases).
- Employers with 500 or more employees must pay the employee’s salary up to $1400 per week during the entire period of removal, until the employee meets the return-to-work criteria described below.
- Employers with more than 10 employees must also continue to provide the benefits to which the employee is normally entitled (e.g., employer-sponsored health insurance) during the removal period.
In each scenario, the employer is not required to provide overtime pay, even if the employee had regularly worked overtime hours in recent weeks. In addition, if the employee receives compensation for lost earnings from any other source, such as employer-paid sick leave, administrative leave or a publicly funded compensation program, then the employer may reduce the amount paid to the removed employee by however much the employee receives from the outside source.
In addition, the obligation to pay MRP benefits ceases when the employee meets the ETS return criteria, even when employers choose to require a longer removal period.
Please note that businesses with fewer than 500 employees may be eligible for refundable tax credits under the American Rescue Plan (ARP) if they provide paid time off for sick and family leave to their employees due to COVID-19-related reasons. The ARP tax credits are available to eligible employers that pay sick and family leave for qualified leave from April 1, 2021, through Sept. 30, 2021. More information is available from the IRS.
Return to Work
Employers must make return-to-work decisions in accordance with guidance from a licensed healthcare provider or applicable guidance from the CDC, which is incorporated by reference in the ETS, unless state or local public health authorities specify a longer period of removal.
However, OSHA recognizes that the CDC’s Strategies to Mitigate Healthcare Personnel Staffing Shortages allows elimination of quarantine for certain health care workers, but only as a last resort, if the workers’ absence would mean there are no longer enough staff to provide safe patient care, specific other amelioration strategies have already been tried, patients have been notified and workers are utilizing additional PPE at all times.
Vaccinations
Employers must support COVID-19 vaccinations for each employee by providing reasonable time and paid leave (for example, paid sick leave, administrative leave) to each employee for vaccination and any side effects experienced following vaccination.
Training
Employers must ensure that each employee receives training, in a language and at a literacy level the employee understands, so the employee comprehends at least the following:
- How the COVID-19 disease is transmitted (including pre-symptomatic and asymptomatic transmission), the importance of hand hygiene to reduce the risk of spreading COVID-19 infections, ways to reduce the risk of spreading COVID-19 through the proper covering of the nose and mouth, the signs and symptoms of the disease, risk factors for severe illness and when to seek medical attention;
- Employer-specific policies and procedures on patient screening and management;
- Tasks and situations in the workplace that could result in COVID-19 infection;
- Workplace-specific policies and procedures to prevent the spread of COVID-19 that are applicable to the employee’s duties (for example, policies on Standard and Transmission-Based Precautions, physical distancing, physical barriers, ventilation, aerosol-generating procedures);
- Employer-specific multi-employer workplace agreements related to infection control policies and procedures, the use of common areas, and the use of shared equipment that affect employees at the workplace;
- Employer-specific policies and procedures for PPE worn to protect against COVID-19, including when PPE is required; limitations of PPE for protection; how to properly put on, wear, take off, care for, store, clean, maintain and dispose of PPE, and any modifications to donning, doffing and cleaning;
- Storage, maintenance and disposal procedures needed to address COVID-19 when PPE is worn, to address workplace hazards other than COVID-19;
- Workplace-specific policies and procedures for cleaning and disinfection;
- Employer-specific policies and procedures on health screening and medical management;
- Available sick leave policies, any COVID-19-related benefits to which the employee may be entitled under applicable federal, state, or local laws, and other supportive policies and practices (for example, telework, flexible hours);
- The identity of the safety coordinators specified in the COVID-19 plan;
- How the employee can obtain copies of this section and any employer-specific policies and procedures developed under this section, including the employer’s written COVID-19 plan, if required.
Employers can rely on training that has been completed prior to the effective date of the ETS as long as it meets the relevant training requirements. Employees must receive additional training whenever changes occur that affect an employee’s risk of contracting COVID-19 at work (for example, new job tasks), policies and procedures are changed or there is an indication that the employee has not retained the necessary understanding or skill.
Employers must ensure that the training is overseen or conducted by a person knowledgeable in the covered subject matter as it relates to the employee’s job duties. The training provided must provide an opportunity for interactive questions and answers with a person knowledgeable in the covered subject matter as it relates to the employer’s job duties.
Anti-Retaliation
Employers must inform each employee that they have a right to the protections required by the ETS and that employers are prohibited from discharging or in any manner discriminating against any employee for exercising their right to the protections required by this section. Employers must not discharge or in any way discriminate against any employee for exercising their right to the protections required by the ETS or for engaging in actions that are required by the ETS.
In addition, section 11(c) of the OSH Act also prohibits employers from discriminating against an employee for exercising rights under, or as a result of actions that are required by, this section. That provision of the Act also protects the employee who files a safety and health complaint, or otherwise exercises any rights afforded by the OSH Act.
Recordkeeping and Reporting
Employers with ten or more employees on the effective date of the ETS must:
- Retain all versions of the COVID-19 plan implemented to comply with this section while this section remains in effect.
- Establish and maintain a COVID-19 log to record each instance identified by the employer in which an employee is COVID-19 positive, regardless of whether the instance is connected to exposure to COVID-19 at work.
The COVID-19 log must contain, for each instance:
- The employee’s name;
- The employee’s contact information;
- The employee’s occupation;
- The location where the employee worked;
- The date of the employee’s last day at the workplace;
- The date of the positive test for, or diagnosis of, COVID-19; and
- The date the employee first had one or more COVID-19 symptoms, if any were experienced.
The information in the COVID-19 log must be recorded within 24 hours of the employer learning that the employee is COVID-19 positive and must be maintained as though it is a confidential medical record and must not be disclosed except as required by the ETS or other federal law. The COVID-19 log must be maintained and preserved while this section remains in effect. The COVID-19 log is intended to assist employers with tracking and evaluating instances of employees who are COVID-19 positive without regard to whether those employees were infected at work. The tracking will help evaluate potential workplace exposure to other employees.
Availability of Records
By the end of the next business day after a request, employers must provide, for examination and copying:
- All versions of the written COVID-19 plan to any employees, their personal representatives, and their authorized representatives.
- The individual COVID-19 log entry for a particular employee to that employee and to anyone having written authorized consent of that employee.
- A version of the COVID-19 log that removes the names of employees, contact information, and occupation, and only includes, for each employee in the COVID-19 log, the location where the employee worked, the last day that the employee was at the workplace before removal, the date of that employee’s positive test for, or diagnosis of, COVID-19, and the date the employee first had one or more COVID-19 symptoms, if any were experienced, to any employees, their personal representatives, and their authorized representatives.
- All records required to be maintained by this section to the Assistant Secretary of OSHA.
Employers with 10 or fewer employees on the effective date of this section are not required to comply with these requirements.
Employers must continue to record all work-related confirmed cases of COVID-19 on their OSHA Forms 300, 300A and 301, or the equivalent forms, if required to do so under OSHA’s recordkeeping requirements.
Reporting COVID-19 Fatalities and Hospitalizations
Employers must report to OSHA each work-related COVID-19 fatality within eight hours of the employer learning about the fatality. Each work-related COVID-19 inpatient hospitalization must be reported to OSHA within 24 hours of the employer learning about the inpatient hospitalization.
When reporting COVID-19 fatalities and inpatient hospitalizations to OSHA in accordance with this section, the employer must follow the requirements in 1904.39, except for 29 CFR part 1904.39(a)(1) and (2) and (b)(6).
Mini Respiratory Protection Program
The mini respiratory protection program (29 CFR 1910.504) is a section of the COVID-19 ETS. It applies only in certain circumstances specified under the ETS, generally when workers are not exposed to suspected or confirmed sources of COVID-19 but where respirator use could offer enhanced worker protection. The mini respiratory protection program provides a limited set of requirements for the safe use of respirators.
OSHA’s normal respiratory protection standard (29 CFR 1910.134) still applies to:
- Any other workplace hazards that might require respiratory protection (e.g., respirable crystalline silica, asbestos or airborne infectious agents such as Mycobacterium tuberculosis)
Respirators can be an effective method of protection against COVID-19 hazards when properly selected and worn. Respirator use is encouraged to provide an additional level of comfort and protection for workers even in circumstances that do not require a respirator to be used. However, if a respirator is used improperly or not kept clean, the respirator itself can become a hazard to the worker. If your employer allows you to provide and use your own respirator, you need to take certain precautions to be sure that the respirator itself does not present a hazard. You should do the following:
- Read and follow all instructions provided by the manufacturer on use, maintenance, cleaning and care, and warnings regarding the respirator’s limitations.
- Keep track of your respirator so that you do not mistakenly use someone else’s respirator.
- Do not wear your respirator where other workplace hazards (for example, chemical exposures) require use of a respirator. In such cases, your employer must provide you with a respirator that is used in accordance with OSHA’s respiratory protection standard (29 CFR part 1910.134).
Employer-provided Respirators
When employers provide employees with respirators, employers must ensure that each employee wearing a respirator receives training prior to first use and if they change the type of respirator, in a language and at a literacy level the employee understands. Employers must make sure their employees at a minimum comprehend the following:
- Training on how to inspect, put on, remove and use a respirator;
- The limitations and capabilities of the respirator, particularly when the respirator has not been fit tested;
- Procedures and schedules for storing, maintaining and inspecting respirators;
- How to perform a user seal check under the mini respiratory protection program; and
- How to recognize medical signs and symptoms that may limit or prevent the effective use of respirators and what to do if the employee experiences signs and symptoms.
Employers must ensure that each employee who uses a tight-fitting respirator performs a user seal check to ensure that the respirator is properly sealed to the face each time the respirator is put on. Acceptable methods of user seal checks include:
- Positive pressure user seal check by trying to blow air out.
- Negative pressure user seal check by sucking air in.
Employers must ensure that each employee corrects any problems discovered during the user seal check. In the case of either type of user seal check (positive or negative), if air leaks around the nose, the employee should use both hands to readjust how the respirator sits on their face or adjust the nosepiece, if applicable. The employee should readjust the straps along the sides of their head until a proper seal is achieved.
When employees are required to wear a respirator and a problem with the seal check arises due to interference with the seal by an employee’s facial hair, employers may provide a different type of respirator to accommodate employees who cannot trim or cut facial hair due to religious belief.
Employers must ensure that a filtering facepiece respirator used by a particular employee is only reused by that employee, and only when:
- The respirator is not visibly soiled or damaged;
- The respirator has been stored in a breathable storage container for at least five calendar days between use and has been kept away from water or moisture;
- The employee does a visual check in adequate lighting for damage to the respirator’s fabric or seal;
- The employee successfully completes a user seal check;
- The employee uses proper hand hygiene before putting the respirator on and conducting the user seal check; and
- The respirator has not been worn more than five days total.
The reuse of single-use respirators is discouraged. Employers must ensure that an elastomeric respirator or power air-purifying respirator (PAPR) is only reused when:
- The respirator is not damaged;
- The respirator is cleaned and disinfected as often as necessary to be maintained in a sanitary condition in accordance with the respiratory protection program (29 CFR 1910.134) and appendix B-2; and
- A change schedule is implemented for cartridges, canisters or filters.
Employers must require employees to discontinue use of a respirator when either the employee or a supervisor reports medical signs or symptoms (for example, shortness of breath, coughing, wheezing, chest pain, any other symptoms related to lung problems, cardiovascular symptoms) that are related to ability to use a respirator. Any employee who previously had a medical evaluation and was determined to not be medically fit to wear a respirator must not be provided with a respirator under this standard unless they are reevaluated and medically cleared to use a respirator.
The mini respiratory protection program is effective as of the date the ETS is published in the Federal Register.
Source: Occupational Safety and Health Administration
The HOTCOMP Safety Committee meets twice a year to discuss the issues of safety in our member hospitals and what we can do to do to help make them safer workplaces. The majority of the Committee members are administrators and safety specialists in your fellow member hospitals. We understand that issues come up through the year. If you would like to post a question to the safety committee members as a group or individuals, please email us at safety@hotcomp.net. We will pass your questions on to the appropriate member(s).
Barry Couch
Board Member,
Program Administrator,
Safety Committee MemberBrian Roland
CEO
Stephens Memorial Hospital
Safety Committee MemberGayle Cannon
Director of HR
Childress Regional
Medical Center
Safety Committee MemberFay Bennett
VP of Employee Services
Guadalupe Regional
Medical Center
Safety Committee MemberBill Hamlyn
Nursing AVP
Oakbend Medical Center
Safety Committee MemberGerardo Garcia
Chief Quality Officer
Childress Regional
Medical Center
Safety Committee MemberAlexander Trudeau
Senior Agency Operations Specialist
Texas Mutual Insurance Company
Advisor, Safety Committee Member
Carol Villareal
HR Manager
Gonzales Healthcare System
Safety Committee MemberJill Smith
Sr. Director of Human Resources
Titus Regional
Medical Center
Safety Committee MemberStacy Rose
Manager of Safety Services
Texas Mutual Insurance Company
Advisor, Safety Committee
Why Your Safety Matters:
You’re receiving this email as a member of the HOTComp safety group. The group is a joint effort between HealthSure and Texas Mutual Insurance Company.
Group members receive exclusive benefits like targeted safety resources, a discount on their workers’ compensation insurance and potential dividends based upon the safe performance of the group. HOTComp group participants have shared in over $3.4 million in group dividends since 2008 in addition to individual dividends from Texas Mutual.
Circumstances under the ETS when workers are exposed to suspected or confirmed sources of COVID-19 - Any other workplace hazards that might require respiratory protection (e.g., respirable crystalline silica, asbestos or airborne infectious agents such as Mycobacterium tuberculosis)
OSHA’s COVID-19 Healthcare Emergency Temporary Standard
COVID-19 Healthcare Worksite Checklist & Employee Job Hazard Analysis
Keep an eye out for your dividend check! The checks have been sent. If you have not received your dividend check contact your Account Executive/Account Manager.
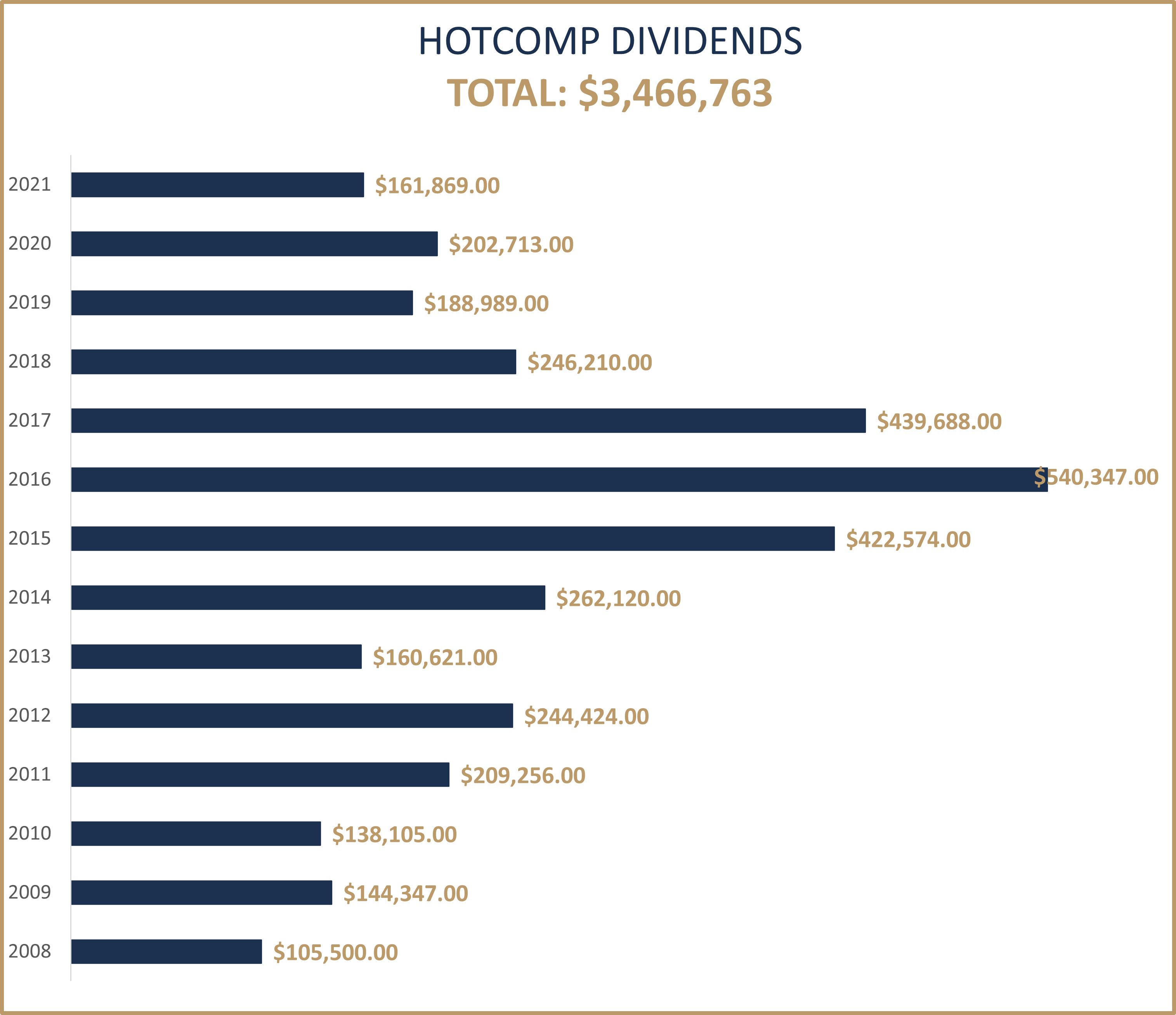
This year marks the thirteenth in a series of safety group dividend payments from Texas Mutual Insurance Company.* Recently the Hospitals of Texas safety group (HOTCOMP) has received $161,869 in dividends. The dividend was earned based on the group members’ dedication to making safety a priority in their hospitals and therefore keeping the group’s loss ratio low. This year marks a total dividend payout to our members since the inception in 2008 of $3,466,763!
Since 1999, Texas Mutual has distributed more than $150 million in safety group dividends among qualifying safety groups. Since that time, Texas Mutual has distributed more than $3.4 billion in both safety group and individual policyholder dividends.
In addition to potential dividends, HOTCOMP safety group members also receive discounts on their workers’ compensation premiums and have access to free workplace safety materials designed for Texas Hospitals.
“Texas Mutual safety services offers valuable information that helps keep hospital employees safe,” said Barry Couch, program manager. “It’s great to know that Texas Mutual is in HotComp’s corner with safety tips and dividends that help hospitals keep costs low and focus on delivering quality care.”
While Texas Mutual has awarded dividends each year since 1999, they are based on performance and therefore are not guaranteed. These dividends are based on the group’s loss history rather than the hospital’s individual history. Hospital members continuously make efforts to reduce claims and improve employee safety measures, assuring that the dividend potential remains for the HOTComp program.
Additionally, dividends must comply with Texas Department of Insurance regulations.
*The dividend calculation period is 18, 30, and 42 months after the group anniversary inception date. There have been a few times during 18 month calculation period, HOTCOMP did not qualify for dividends due to a high loss ratio.
OSHA’s COVID-19 Healthcare Emergency Temporary Standard
OSHA’s COVID-19 Healthcare Emergency Temporary Standard
On June 10, 2021, the Occupational Health and Safety Administration (OSHA) announced its COVID-19 Healthcare Emergency Temporary Standard (ETS). The ETS was developed to protect health care and health care support service workers from occupational exposure to COVID-19 in settings where people with COVID-19 are reasonably expected to be present. The ETS is effective June 21, 2021.
Covered employers include hospitals, nursing homes and assisted living facilities; emergency responders; home health care workers and employees in ambulatory care settings where suspected or confirmed coronavirus patients are treated.
The ETS requires covered health care employers to develop and implement a COVID-19 plan to identify and control COVID-19 hazards in the workplace and encourage vaccinations and respirator use when needed. This Compliance Bulletin reviews the requirements of the OSHA COVID-19 ETS for health care.
Action Steps
Health care employers should familiarize themselves with OSHA’s new COVID-19 ETS. Employers subject to the ETS requirements must implement all policies, measures and procedures necessary for compliance with the new standard. Employers are encouraged to visit OSHA’s COVID-19 Healthcare ETS website for compliance guidance and resources.
Employers should continue to monitor OSHA communications for updates on workplace safety and health issues.
Employers Subject to the ETS
The ETS applies to all settings where employees provide health care services or health care support services, except for:
OSHA does not intend to preclude employers of employees who are unable to be vaccinated from the scope of the well-defined hospital ambulatory care and home health care settings. Under various anti-discrimination laws, workers who cannot be vaccinated because of medical conditions, such as allergies to vaccine ingredients, or certain religious beliefs may ask for a reasonable accommodation from their employer. Accordingly, where an employer reasonably accommodates an employee who is unable to be vaccinated in a manner that does not expose the employee to COVID-19 hazards (for example telework or working in isolation), that employer may be within the exemption of the well-defined hospital ambulatory care and home health care settings.
Where a health care setting is embedded within a non-health care setting (such as a medical clinic in a manufacturing facility or a walk-in clinic in a retail setting), the health care section of the ETS applies only to the embedded healthcare setting and not to the remainder of the physical location. Where emergency responders or other licensed health care providers enter a non-health care setting to provide health care services, this section applies only to the provision of the health care services by that employee (emergency responders or other licensed health care providers).
However, personal protective equipment (PPE), physical distancing and physical barriers do not apply to employees who are fully vaccinated in well-defined areas where there is no reasonable expectation that any person with suspected or confirmed COVID-19 will be present.
Finally, the implementation of ETS requirements, with the exception of any employee self-monitoring conducted before the start of each work day and shift, must be at no cost to employees. State or local government mandates or guidance still apply even if those requirements go beyond the requirements of the ETS, but they must not be inconsistent with the ETS.
COVID-19 Plan
Employers must develop and implement a COVID-19 plan for each workplace. Employers with more than 10 employees are required to have a written COVID-19 plan. Employers with multiple workplaces that are substantially similar may develop their COVID-19 plans by workplace type, rather than by individual workplace, so long as all required site-specific information is included in the plan.
Employers must designate one or more workplace COVID-19 safety coordinators to implement and monitor the COVID-19 plan developed under the ETS. The COVID-19 safety coordinator must be knowledgeable in control principles and practices as they apply to the workplace and employee job operations. The identity of the safety coordinator must be documented in any written COVID-19 plan. The safety coordinator must have the authority to ensure compliance with all aspects of the COVID-19 plan.
Employers must conduct a workplace-specific hazard assessment to identify potential workplace hazards related to COVID-19. In order for an employer to be exempt from providing controls in a well-defined area with fully vaccinated employees, the COVID-19 plan must include policies and procedures to determine an employee’s vaccination status.
Employers must seek input and involvement of non-managerial employees and their representatives in the hazard assessment and during the development and implementation of their COVID-19 plan. Employers must monitor each workplace to ensure the ongoing effectiveness of their COVID-19 plans and update them as needed. COVID-19 plans must address the hazards identified by the assessment and include policies and procedures to:
Employers must develop and implement policies and procedures to adhere to the U.S. Centers for Disease Control and Prevention’s (CDC) Guidelines for Isolation Precautions.
Patient Screening and Management
In settings where direct patient care is provided, employers must:
Employers are encouraged to use telehealth services where available and appropriate in order to limit the number of people entering the workplace.
PPE Requirements
Employers are required to provide, and ensure that employees wear, facemasks (surgical, medical procedure, dental or isolation masks that are approved by the Food and Drug Administration and wear them over their mouth and nose when indoors or occupying a vehicle with other people for work purposes.
Employees must change their facemasks at least once per day—or more frequently, as necessary, whenever they are soiled or damaged. Employers must provide a sufficient number of facemasks so employees can change facemasks as required.
Exceptions
Exceptions to the facemask requirements include:
Employers may determine that the use of face shields, without facemasks, in certain settings is not appropriate due to other infection control concerns. Where a face shield is required, employers must ensure that face shields are cleaned at least daily and are not damaged. When employees bring their own face shields, employers may allow them to use them and employers are not required to reimburse the employees for those face shields.
PPE During COVID-19 Exposure
When employees are exposed to a person with suspected or confirmed COVID-19, or for aerosol-generating procedures performed on a person with suspected or confirmed COVID-19, employers must provide:
When there is a limited supply of filtering facepiece respirators, employers may follow CDC’s Strategies for Optimizing the Supply of N95 Respirators.
Employers may provide respirators to their employees instead of a facemask as required by the ETS. In such circumstances, employer must also comply with the ETS mini respiratory protection program (§ 1910.504). In addition, employers must provide protective clothing and equipment (respirators, gloves, gowns, goggles, face shields) to each employee in accordance with the standard and transmission-based precautions in health settings in accordance with the CDC’s Guidelines for Isolation Precautions.
Aerosol-generating Procedures for Suspected or Confirmed COVID-19
When an aerosol-generating procedure is performed on a person with suspected or confirmed COVID-19, employers must:
Physical Distancing and Barriers
Employers must ensure that each employee is separated from other people by at least six feet when indoors unless they can demonstrate that such physical distancing is not feasible for a specific activity. This requirement does not apply to momentary exposure while people are in movement (passing in hallways or aisles).
When establishing six feet of physical distancing is not possible, employers must ensure that their employees are as far apart as possible from all other employees. OSHA suggests that physical distancing can be achieved through any or all of the following measures:
At each fixed work location outside of direct patient care areas (entryway/lobby, check-in desk, triage, hospital pharmacy windows, bill payment) where each employee is not separated from all other people by at least six feet, employers must install cleanable or disposable solid barriers. An exception is possible for employers that can demonstrate that installing barriers is not feasible. Barriers must be sized and located to block face-to-face pathways between individuals, based on where each person would normally stand or sit. The barrier may have a pass-through space at the bottom for objects and merchandise. Physical barriers are not required in direct patient care areas or resident rooms.
Cleaning and Disinfection
In patient care areas, resident rooms and for medical devices and equipment, employers must follow standard practices for cleaning and disinfecting surfaces and equipment in accordance with the CDC’s COVID-19 Infection Prevention and Control Recommendations and the Guidelines for Environmental Infection Control.
In all other areas, employers must:
Employers must provide alcohol-based hand rub that is at least 60 percent alcohol, or provide readily accessible hand washing facilities.
Ventilation
Employers that own or control buildings or structures with existing heating, ventilation and air conditioning (HVAC) systems must ensure that:

